As the dilemma of “surprise billing” at hospitals around the nation gains scrutiny from the White House and Congress, many major hospital groups indicated they want a hand in shaping the conversation. In a letter sent to the Congressional leaders, from the American Hospital Association and the Federation of American Hospitals, laid out principles they want legislators to consider as they seek to address the problem. Their solutions aimed at policies for health payers and asked for protection for the patients. Notably, however, they also opposed the controversial practice of balance billing by providers.
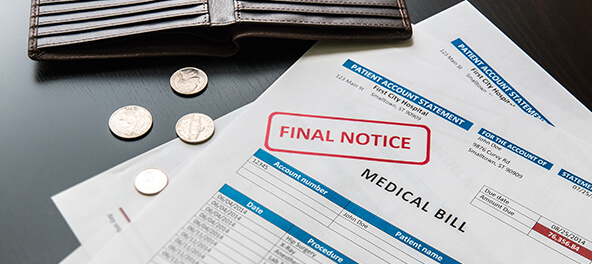
These “surprise bills” or “balance bills” can devastate patients. Every little thing can be charged because a patient needed emergency help, but they were at an out of network hospital or received surgery from an out of network doctor. The bill can skyrocket and leave the patient in a financial crisis. This issue has created a “back and forth” in the industry over who is to blame for the surprise medical bills or the practice of charging patients for care that is more costly than the actual amount or not covered by their insurance. A group of insurance, business, and consumer groups announced in December that they would band together to push for stronger patient protections and released their principles for the conversation.
The letter from the hospital groups stated, “We are fully committed to protecting patients from “surprise bills” that result from unexpected gaps in coverage or medical emergencies.” This also included America’s Essential Hospitals, the Association of American Medical Colleges, the Catholic Health Association of the United States and the Children’s Hospital Association. They added, “We appreciate your leadership on this issue and look forward to continuing to work with you on a federal legislative solution.”
The group wants a definition of “surprise bills” agreed upon, and under this definition, call for more financial help to the patient. They also want protection for patients who are denied payment by a payer if, for example, the health plan determines the instance was not an emergency. Another massive principle pushed for is ensuring patients have access to comprehensive provider networks and accurate network information through their health plans. The “surprise bill” is something that happens one out of every five medical emergencies that take place. For the sake of the patient, it should be a priority to solve these issues and form a resolution.
![]()